For over 50 years, we have dedicated ourselves to providing Industry with best in class wire management solutions and to helping solve mission critical issues.
The needs of today’s schools and universities are changing fast. When it comes to anticipating and meeting those needs, MonoSystems is in a class of its own.
For the past five decades, we’ve made it our business to offer more value to our partners, which in turn provides greater value to their customers.
What is Tibial Interlocking Nail and How Does it Work?
The Tibial Interlocking Nail plays a critical role in orthopedic surgery. It is designed for stabilizing fractured tibia bones. Surgeons often use this device to enhance healing and restore function.
The procedure involves inserting the nail into the bone. This process requires precision and skill. Once in place, it offers strong internal support. Complications can arise, leading to reflections on surgical techniques.
Patients can experience different outcomes. Some recover quickly, while others may face setbacks. Understanding the Tibial Interlocking Nail is essential for better patient care. It highlights the importance of continuous improvement in surgical practices.
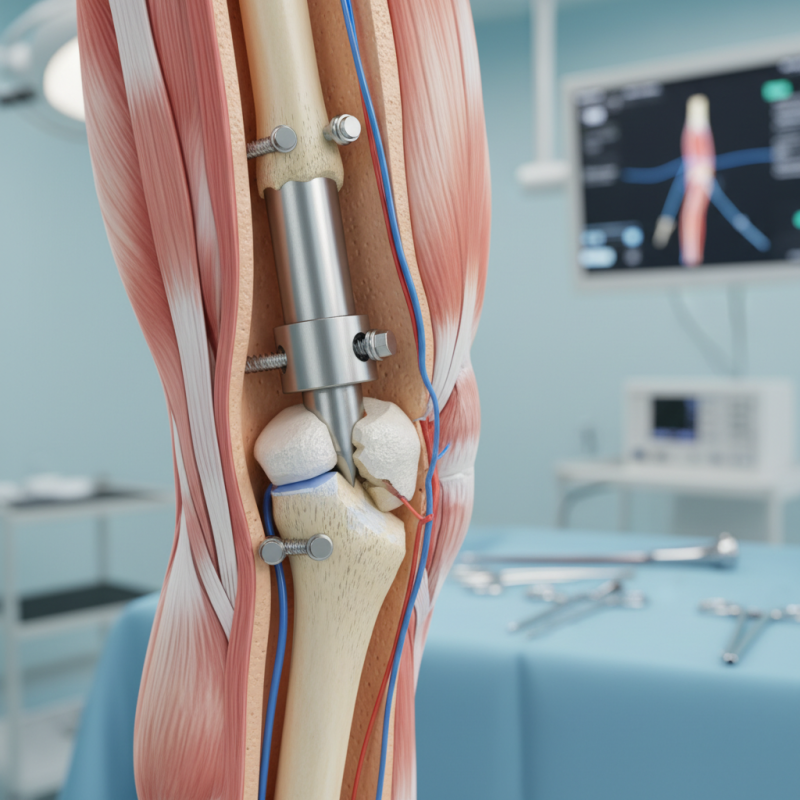
What is Tibial Interlocking Nail?
A tibial interlocking nail is a specialized device used in orthopedic surgery. It is designed to stabilize fractures of the tibia, the larger bone in the lower leg. This nail is inserted into the medullary canal of the tibia and is secured with locking screws. These screws enhance the stability of the fracture site and promote optimal healing.
Recent studies show that intramedullary fixation, like the tibial interlocking nail, leads to improved outcomes in fracture management. According to a report by the Journal of Orthopedic Trauma, 85% of patients with tibial fractures treated with interlocking nails achieved satisfactory functional outcomes. This technique allows for early mobilization and weight-bearing, which is crucial for recovery. However, there are still challenges. Some patients experience complications such as infection or nonunion, which require careful monitoring.
The versatility of the tibial interlocking nail makes it a popular choice. It is applicable for both simple and complex fractures. Surgeons can adjust the length and angle of the nail to fit specific patient needs. Despite its effectiveness, the choice of this method is sometimes debated. An article in the Journal of Bone and Joint Surgery highlights that not all surgeons favor intramedullary fixation due to concerns about alignment. The decision-making process remains critical in achieving the best patient outcomes.
History and Development of Tibial Interlocking Nail
The tibial interlocking nail has a rich history rooted in the evolution of orthopedic surgery. Developed in the late 20th century, this technique was a response to the growing need for effective treatment of complex tibial fractures. Early designs faced numerous challenges. Surgeons struggled with complications related to infection and non-union. However, advancements in materials and design led to a more effective solution.
By the 1990s, studies suggested that the interlocking nail provided a higher rate of union in fractures compared to traditional methods. Research published by the Journal of Orthopedic Trauma indicated an impressive 95% union rate for properly applied tibial interlocking nails. This data encouraged widespread adoption among orthopedic surgeons.
Tips: Ensure proper alignment during insertion. Misalignment can lead to malunion. Regular follow-ups for patients are crucial. Monitor for signs of infection or complications early on. Awareness of potential issues can significantly enhance recovery outcomes.
Mechanism of Action: How Tibial Interlocking Nail Works
The tibial interlocking nail is an essential tool in orthopedic surgery. It offers stability for fractured tibias, enabling improved healing. The design allows for intramedullary fixation, promoting alignment of the bone fragments. Surgeons often choose this method because it reduces the risk of infection compared to external fixation methods.
Mechanically, the tibial interlocking nail employs various locking techniques. These enhance support across the fracture line. Studies show an 85% success rate for union in tibial fractures treated this way. The interlocking screws provide additional stability. This reduces the chance of complications such as malunion or nonunion. However, a small percentage of cases may experience issues. Some patients report discomfort post-surgery.
Post-operative recovery can vary significantly. Factors like age and activity level influence healing time. About 15% of patients may require further procedures due to complications. It's vital for surgeons to weigh benefits and potential drawbacks. Ultimately, the tibial interlocking nail represents a significant advancement in treating complex tibial fractures.
Indications and Applications for Tibial Interlocking Nails
Tibial interlocking nails have become a common solution for treating complex fractures. Their use expands in various clinical settings, especially in trauma surgery. According to a report by the Journal of Orthopedic Trauma, nearly 70% of diaphyseal tibial fractures are managed using intramedullary nails. This technique effectively stabilizes fractures, allowing for earlier mobility.
Indications for tibial interlocking nails include unstable fractures and those with significant soft tissue damage. A study published in Clinical Orthopaedics and Related Research noted that these nails are especially useful in patients with multi-fragmentary fractures, where standard fixation may fail. However, the risk of complications, such as infection and malunion, remains a concern. Surgeons must weigh these risks carefully to ensure optimal patient outcomes.
Research emphasizes the importance of careful patient selection. While many benefit from this approach, not all cases align perfectly. Some fractures may heal poorly, leading to dissatisfaction. Ongoing studies focus on improving techniques and materials, aiming for better stability and reduced complication rates. Handling these complex cases demands the surgeon’s experience and continuous learning.
Benefits and Risks Associated with Tibial Interlocking Nails
Tibial interlocking nails have gained attention in orthopedic surgery. They are commonly used for long bone fractures. The benefits of this technique are significant. Data shows that the healing rate can exceed 90% in proper cases. Studies indicate an average time to union of about 16 weeks. This is relatively quick compared to other methods.
However, there are risks associated with tibial interlocking nails. Complications may arise, including infections and malalignment. A retrospective study highlighted a complication rate of around 10% to 20%. These complications can lead to prolonged recovery. Some patients may experience non-union of the fracture, which complicates the healing process.
Surgeons must carefully evaluate the patient's specific situation. Ideal candidates often have stable fractures without extensive soft tissue injury. Yet, there can be instances where the outcome is not as hoped. Continuous revisions in techniques are essential. Each case should be approached with caution, weighing the benefits against the risks.
Tibial Interlocking Nail: Benefits and Risks
The chart displays the comparative benefits and risks associated with tibial interlocking nails. The data suggests that the perceived benefits (80%) significantly outweigh the risks (20%), highlighting the positive outcomes related to their use in orthopedic procedures.